Your healthcare data strategy goes far beyond simple data management. It's the blueprint that unites your teams, workflows, and systems toward common objectives. Execute it well, and you'll turn fragmented information into a strategic advantage that enhances patient outcomes, cuts operational costs, and fuels breakthrough innovations.
In this post, we'll cover:
- Why Your Current Approach Isn't Working (And What's at Stake)
- The 6 Pillars of a Winning Healthcare Data Strategy
- How to Build Momentum Without Getting Stuck in Analysis Paralysis
- A Practical Implementation Roadmap That Actually Works
Why Healthcare Data Strategy Matters More Than Ever
Let's be honest: most healthcare organizations are sitting on a goldmine of data they can't effectively use.
You've got clinical teams pulling reports from one system, finance working from another, and operations creating their own spreadsheets because nobody trusts the "official" numbers. Meanwhile, compliance is breathing down your neck, and executives are asking for insights you simply can't provide quickly or accurately.
The hidden costs of fragmented data:
- Medical errors increase when critical information is scattered across systems
- Staff waste hours reconciling conflicting reports instead of focusing on patient care
- Compliance violations happen when audit trails are incomplete or inconsistent
- Strategic decisions get delayed because no one can agree on what the data actually says
But here's what organizations with strong data strategies achieve:
- 15% reduction in diagnostic errors through better data integration
- 20% improvement in operational efficiency by eliminating manual workarounds
- 30% faster decision-making when leadership has access to trusted, real-time insights
- Significant cost savings from reduced redundancy and improved resource allocation
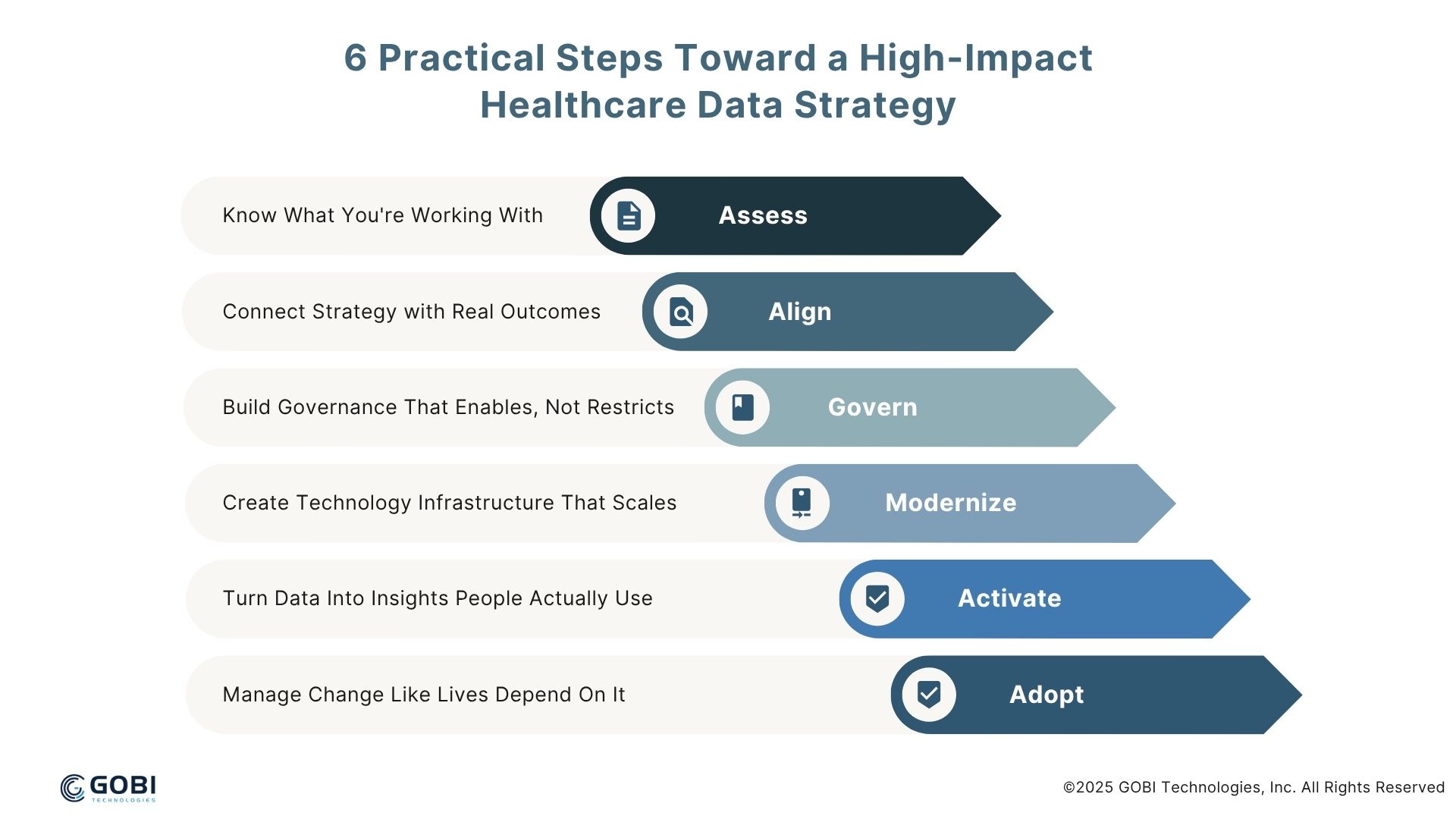
6 Practical Steps Toward a High-Impact Healthcare Data Strategy
A successful healthcare data strategy rests on six foundational pillars. Miss any one of them, and your entire initiative risks collapse.
1. Know What You're Working With: Data Landscape Assessment
You can't fix what you can't see. Before you build anything new, you need a complete picture of your current data ecosystem.
What this looks like in practice:
- Map every data source across clinical, operational, and financial systems
- Identify where the same information lives in multiple places (and why the numbers don't match)
- Document data flows between systems and departments
- Assess data quality: missing fields, duplicates, outdated records, inconsistent formats
Pro tip: Start with your most critical use cases. If you're focused on reducing readmissions, trace the data journey from admission to discharge to follow-up. Don't try to map everything at once.
2. Align Strategy with Real Outcomes
Your data strategy must serve your organization's mission, not the other way around.
Too many healthcare organizations start with technology and try to figure out the use cases later. That's backwards. Start with the outcomes that matter most to your patients and your bottom line.
Questions to ask:
- What are our top 3 clinical quality improvement priorities?
- Which operational inefficiencies cost us the most time and money?
- What strategic initiatives depend on better data and analytics?
- How do we measure success in patient satisfaction, safety, and outcomes?
Tie everything back to measurable goals:
- Reduce hospital-acquired infections by 25%
- Improve patient satisfaction scores by 15%
- Decrease average length of stay by 0.5 days
- Increase staff productivity by 20%
3. Build Governance That Enables, Not Restricts
Healthcare data governance isn't about creating more bureaucracy — it's about building trust and ensuring compliance while keeping data accessible to those who need it.
Your governance framework should address:
- Data ownership: Who's responsible for maintaining data quality in each system?
- Access controls: What data can different roles access, and under what circumstances?
- Quality standards: How do you define "good" data, and how do you measure it?
- Compliance requirements: How do you stay current with HIPAA, state regulations, and other requirements?
Make governance practical:
- Create clear escalation paths when data quality issues arise
- Implement automated quality checks that catch problems before they reach end users
- Establish data stewards in each department who understand both clinical workflows and data requirements
- Regular audits that identify gaps before they become compliance issues
4. Create Technology Infrastructure That Scales
Your technology stack should make data integration easier, not harder. If you're still building point-to-point connections between every system, you're setting yourself up for maintenance nightmares.
Key architectural principles:
- Centralized data repository: Whether it's a data warehouse, data lake, or hybrid approach, you need a single source of truth
- Standardized interfaces: Use APIs and industry standards like HL7 FHIR to connect systems
- Cloud-first approach: Scalability and flexibility matter more than owning hardware
- Security by design: Encryption, access controls, and audit logging built into every layer
Don't over-engineer: Start with proven technologies that solve your immediate needs. You can always add sophistication later.
5. Turn Data Into Insights People Actually Use
Raw data is worthless if it doesn't lead to better decisions. Your analytics capabilities should match your organization's maturity level and provide insights that drive action.
Start with the basics:
- Descriptive analytics: What happened? Real-time dashboards for key metrics
- Diagnostic analytics: Why did it happen? Root cause analysis for quality issues
- Predictive analytics: What's likely to happen? Models for patient risk, resource needs, demand forecasting
Make analytics actionable:
- Embed insights into existing workflows rather than creating separate reporting systems
- Focus on metrics that lead to specific actions, not just interesting observations
- Provide different views for different roles (executives need summaries, clinicians need details)
- Enable self-service analytics with appropriate guardrails
6. Manage Change Like Lives Depend On It (Because They Do)
The best data strategy in the world won't matter if your people won't use it. Healthcare professionals are notoriously resistant to change, especially when it comes to technology that disrupts established workflows.
How to drive adoption:
- Identify clinical champions who can advocate for new tools and processes
- Focus on user experience — if it takes more than three clicks, it won't get used
- Provide comprehensive training that emphasizes patient care benefits, not just technical features
- Start small with pilot programs that demonstrate value before rolling out organization-wide
- Gather feedback continuously and adjust based on real-world usage
How to Build Momentum Without Getting Stuck
The biggest risk to any healthcare data strategy isn't technical failure. It's losing momentum before you can demonstrate value. Here's how to keep moving forward:
Start with High-Impact, Low-Risk Use Cases
Pick your first projects carefully. You want something that:
- Delivers visible value within 90 days
- Doesn't require massive system changes
- Has strong stakeholder support
- Can be replicated in other areas
Examples of good starter projects:
- Automated quality metrics dashboard for infection control
- Predictive analytics for bed management
- Integrated reporting for specific service lines
- Patient flow optimization for emergency departments
Build on Early Wins
Once you've proven value with initial projects, expand systematically:
- Replicate successful use cases in other departments or service lines
- Add complexity gradually — more data sources, advanced analytics, real-time capabilities
- Scale infrastructure as demand grows
- Develop internal expertise through training and hiring
Avoid Common Pitfalls
- Don't try to boil the ocean: Focus on specific problems with clear solutions
- Don't ignore change management: Technical success means nothing without user adoption
- Don't neglect data quality: Garbage in, garbage out still applies
- Don't skip governance: Cutting corners on compliance will cost you later
Your 90-Day Implementation Roadmap
Days 1-30: Foundation Setting
- Assemble your core team (clinical, IT, operations, compliance)
- Complete data landscape assessment for your first use case
- Define success metrics and establish baselines
- Identify quick wins that can demonstrate value
Days 31-60: Pilot Development
- Build basic data integration for your pilot use case
- Create initial analytics and reporting capabilities
- Establish governance processes and security controls
- Begin user training and change management activities
Days 61-90: Pilot Launch and Iteration
- Launch pilot with a small group of engaged users
- Gather feedback and make adjustments
- Measure results against your success metrics
- Plan expansion to additional use cases or departments
The Bottom Line
Healthcare data strategy isn't about having the most sophisticated technology or the largest data warehouse. It's about systematically connecting data to decisions that improve patient care and organizational performance.
The organizations that succeed are those that:
- Start with clear, measurable outcomes
- Build governance that enables rather than restricts
- Focus on user adoption from day one
- Take a systematic approach to scaling capabilities
Your data strategy should be a living document that evolves with your organization's needs and capabilities. The goal isn't perfection — it's progress that delivers real value to patients, providers, and the bottom line.






.webp)

